Calendar-based contraceptive methods
| Calendar-based methods | |
|---|---|
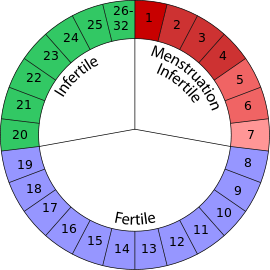 An illustration of the Standard Days Method. This method may be used by women whose menstrual cycles are always between 26 and 32 days in length |
|
| Background | |
| Birth control type | Behavioral |
| First use | Ancient (ad hoc) 1930s (Rhythm method) 1999 (Standard Days) |
| Failure rates (first year) | |
| Perfect use | Standard Days: 5% Rhythm method: 9% |
| Typical use | 25% |
| Usage | |
| Reversibility | Yes |
| User reminders | Dependent upon strict user adherence to methodology |
| Clinic review | None |
| Advantages and disadvantages | |
| STD protection | No |
| Benefits | No side effects, can be used to facilitate pregnancy achievement |
Calendar-based methods are various methods of estimating a woman's likelihood of fertility, based on a record of the length of previous menstrual cycles. Various systems are known as the Knaus–Ogino Method, rhythm method, and Standard Days Method. These systems may be used to achieve pregnancy, by timing unprotected intercourse for days identified as fertile, or to avoid pregnancy, by restricting unprotected intercourse to days identified as infertile.
The first formalized calendar-based method was developed in 1930 by John Smulders, a Roman Catholic physician from the Netherlands. It was based on knowledge of the menstrual cycle which was independently discovered by Hermann Knaus (Austria), and Kyusaku Ogino (Japan). This system was a main form of birth control available to Catholic couples for several decades, until the popularization of symptoms-based fertility awareness methods. A new development in calendar-based methods occurred in 1999, when Georgetown University introduced the Standard Days Method. The Standard Days Method is promoted in conjunction with a product called CycleBeads, a ring of colored beads which are meant to help the user keep track of her fertile and non-fertile days.
Contents |
Terminology
Some sources may treat the terms rhythm method and fertility awareness as synonymous.[1] However, fertility awareness is usually used as a broad term that includes tracking basal body temperature and cervical mucus as well as cycle length. The World Health Organization considers the rhythm method to be a specific type of calendar-based method, and calendar-based methods to be only one form of fertility awareness.[2]
More effective than calendar-based methods, systems of fertility awareness that track basal body temperature, cervical mucus, or both, are known as symptoms-based methods. Teachers of symptoms-based methods take care to distance their systems from the poor reputation of the rhythm method.[3] Many consider the rhythm method to have been obsolete for at least 20 years,[4] and some even exclude calendar-based methods from their definition of fertility awareness.[5]
Some sources may treat the terms rhythm method and natural family planning as synonymous.[6] In the early twentieth century, the calendar-based method known as the rhythm method was promoted by members of the Roman Catholic Church as the only morally acceptable form of family planning. Methods accepted by this church are referred to as natural family planning (NFP): so at one time, the term "the rhythm method" was synonymous with NFP. Today, NFP is an umbrella term that includes symptoms-based fertility awareness methods and the lactational amenorrhea method as well as calendar-based methods such as rhythm.[7] This overlap between uses of the terms "the rhythm method" and "natural family planning" may contribute to confusion.
The term "the rhythm method" is sometimes used, in error, to describe the behavior of any people who have unprotected vaginal intercourse, yet wish to avoid pregnancy.
History
Early methods
It is not known if historical cultures were aware of what part of the menstrual cycle is most fertile. In the year 388, Augustine of Hippo wrote of periodic abstinence. Addressing followers of Manichaeism, his former religion, he said, "Is it not you who used to counsel us to observe as much as possible the time when a woman, after her purification, is most likely to conceive, and to abstain from cohabitation at that time...?"[8] If the Manichaieans practiced something like the Jewish observances of menstruation, then the "time... after her purification" would have indeed been when "a woman... is most likely to conceive."[9] Over a century previously, however, the influential Greek physician Soranus had written that "the time directly before and after menstruation" was the most fertile part of a woman's cycle; this inaccuracy was repeated in the sixth century by the Byzantine physician Aëtius. Similarly, a Chinese sex manual written close to the year 600 stated that only the first five days following menstruation were fertile.[9] Some historians believe that Augustine, too, incorrectly identified the days immediately after menstruation as the time of highest fertility.[10]
Written references to a "safe period" do not appear again for over a thousand years.[9] Scientific advances prompted a number of secular thinkers to advocate periodic abstinence to avoid pregnancy:[11] in the 1840s it was discovered that many animals ovulate during estrus. Because some animals (such as dogs) have a bloody discharge during estrus, it was assumed that menstruation was the corresponding most fertile time for women. This inaccurate theory was popularized by physicians Bischoff, Pouchet, and Adam Raciborski.[9][10] In 1854, an English doctor named George Drysdale correctly taught his patients that the days near menstruation are the least fertile, but this remained the minority view for the remainder of the nineteenth century.[9]
Knaus–Ogino or rhythm method
In 1905 Theodoor Hendrik van de Velde, a Dutch gynecologist, showed that women only ovulate once per menstrual cycle.[12] In the 1920s, Kyusaku Ogino, a Japanese gynecologist, and Hermann Knaus, from Austria, working independently, each made the discovery that ovulation occurs about fourteen days before the next menstrual period.[13] Ogino used his discovery to develop a formula for use in aiding infertile women to time intercourse to achieve pregnancy.
In 1930, John Smulders, a Roman Catholic physician from the Netherlands, used Knaus and Ogino's discoveries to create a method for avoiding pregnancy. Smulders published his work with the Dutch Roman Catholic medical association, and this was the official rhythm method promoted over the next several decades.[13] In 1932 a Catholic physician published a book titled The Rhythm of Sterility and Fertility in Women describing the method,[11] and the 1930s also saw the first U.S. Rhythm Clinic (founded by John Rock) to teach the method to Catholic couples.[14]
Later 20th century to present
In the first half of the twentieth century, most users of the rhythm method were Catholic, they were following their church's teaching that all other methods of birth control were sinful. In 1968 the encyclical Humanae Vitae included the statement, "It is supremely desirable... that medical science should by the study of natural rhythms succeed in determining a sufficiently secure basis for the chaste limitation of offspring." This is interpreted as favoring the then-new, more reliable symptoms-based fertility awareness methods over the rhythm method. Currently, many fertility awareness teachers consider the rhythm method to have been obsolete for at least 20 years,[4] and calendar-based methods are not classified as NFP by the United States Conference of Catholic Bishops.[15]
New attention was drawn to calendar-based methods in 1999, when Georgetown University introduced the Standard Days Method. Designed to be simpler to teach and use than the older rhythm method, the Standard Days Method is being successfully integrated into family planning programs worldwide.
Types and effectiveness
Most menstrual cycles have several days at the beginning that are infertile (pre-ovulatory infertility), a period of fertility, and then several days just before the next menstruation that are infertile (post-ovulatory infertility). The first day of red bleeding is considered day one of the menstrual cycle. To use these methods, a woman is required to know the length of her menstrual cycles.
Imperfect use of calendar-based methods would consist of not correctly tracking the length of the woman's cycles, thus using the wrong numbers in the formula, or of having unprotected intercourse on an identified fertile day. The discipline required to keep accurate records of menstrual cycles, and to abstain from unprotected intercourse, makes imperfect use fairly common. The actual failure rate of calendar-based methods is 25% per year.[16]
Rhythm method (Knaus–Ogino method)
To find the estimated length of the pre-ovulatory infertile phase, nineteen (19) is subtracted from the length of the woman's shortest cycle. To find the estimated start of the post-ovulatory infertile phase, ten (10) is subtracted from the length of the woman's longest cycle.[17] A woman whose menstrual cycles ranged in length from 30 to 36 days would be estimated to be infertile for the first 11 days of her cycle (30-19=11), to be fertile on days 12-25, and to resume infertility on day 26 (36-10=26). When used to avoid pregnancy, the rhythm method has a perfect-use failure rate of up to 9% per year.[16]
Standard Days Method
Developed by Georgetown University's Institute for Reproductive Health, the Standard Days Method has a simpler rule set and is more effective than the rhythm method. A product, called CycleBeads, was developed alongside the method to help the user keep track of estimated high and low fertility points during her menstrual cycle. The Standard Days Method may only be used by women whose cycles are always between 26 and 32 days in length. In this system:
- Days 1-7 of a woman's menstrual cycle are considered infertile
- Days 8-19 are considered fertile
- From Day 20, infertility is considered to resume
When used to avoid pregnancy, the Standard Days Method has a perfect-use failure rate of 5% per year.[18]
Software-based systems
A software program developed in Germany from 1995 to 2001, Perimon is a stricter variant of the rhythm method. It requires a greater period where unprotected sex is not allowed when used to avoid pregnancy, designating a maximum of 10.5 days each cycle as infertile. If 7 of those infertile days occur when a woman's is menstruating, this means there are only 3.5 days of non-menstrual infertile days per cycle.
No clinical studies have been done to determine effectiveness, but the program's developers claim a perfect-use failure rate of 4% per year. The Perimon software requires a paid subscription.[19]
Several Web-based implementations of the cycle method are known. Some websites are also adapted the women who has variant cycle time.[20] More examples can be found at Menstruation at the Open Directory Project.
Advantages
The Standard Days method (SDM) is increasingly being introduced as part of family planning programs in developing countries. The method is satisfactory for many women and men who find other methods unacceptable; offering it through family planning centers results in a significant increase in contraceptive use among couples who do not want to become pregnant.[21][22] The low cost of the method may also enable it to have a significant positive impact in countries that lack funding to provide other methods of birth control.[23]
Potential concerns
Failure rate
One concern related to the use of calendar-based methods is their relatively high failure rate, compared to other methods of birth control. Even when used perfectly, calendar-based methods, especially the rhythm method, result in a high pregnancy rate among couples intending to avoid pregnancy. Of commonly known methods of birth control, only the cervical cap and contraceptive sponge have comparably high failure rates. This lower level of reliability of calendar-based methods is because their formulas make several assumptions that are not always true.[17]
The postovulatory (luteal) phase has a normal length of 12 to 16 days,[24] and the rhythm method formula assumes all women have luteal phase lengths within this range. However, many women have shorter luteal phases, and a few have longer luteal phases.[25] For these women, the rhythm method formula incorrectly identifies a few fertile days as being in the infertile period.[17]
Calendar-based methods use records of past menstrual cycles to predict the length of future cycles. However, the length of the pre-ovulatory phase can vary significantly, depending on the woman's typical cycle length, stress factors, medication, illness, menopause, breastfeeding, and whether she is just coming off hormonal contraception. If a woman with previously regular cycles has a delayed ovulation due to one of these factors, she will still be fertile when the method tells her she is in the post-ovulatory infertile phase. If she has an unusually early ovulation, calendar-based methods will indicate she is still in the pre-ovulatory infertile phase when she has actually become fertile.[17]
Finally, calendar-based methods assume that all bleeding is true menstruation. However, mid-cycle or anovulatory bleeding can be caused by a number of factors.[26] Incorrectly identifying bleeding as menstruation will cause the method's calculations to be incorrect.[17]
Embryonic health
It has been suggested that unprotected intercourse in the infertile periods of the menstrual cycle may still result in conceptions, but create embryos incapable of implanting.[27] It has also been suggested that pregnancies resulting from method failures of periodic abstinence methods are at increased risk of miscarriage and birth defects due to aged gametes at the time of conception.[28] Newer research suggests that timing of conception has no effect on miscarriage rates,[29] low birth weight, or preterm delivery.[30]
References
- ↑ "Rhythm Method". Contraception.net. 2008. http://www.contraception.net/resource_centre/rhythm_method.asp. Retrieved 2008-05-18.
- ↑ Medical Eligibility Criteria for Contraceptive Use:Fertility awareness-based methods. Third edition. World Health Organization. 2004. http://www.who.int/reproductive-health/publications/mec/fab.html. Retrieved 2008-04-29.
- ↑ Weschler, Toni. "Fertility Myths". Ovusoft. Taking Charge of Your Fertility. http://www.ovusoft.com/library/myths.asp#19. Retrieved 2008-04-29.
- ↑ 4.0 4.1 Weschler, Toni (2002). Taking Charge of Your Fertility (Revised ed.). New York: HarperCollins. pp. 3–4. ISBN 0-06-093764-5.
- ↑ Singer, Katie (2007). "What is Fertility Awareness?". The Garden of Fertility. http://www.gardenoffertility.com/fertilityawareness.shtml. Retrieved 2008-05-18.
- ↑ "Rhythm Method". Birth Control Health Center. WebMD. 2005. http://www.webmd.com/sex/birth-control/rhythm-method. Retrieved 2008-05-18.
- ↑ "Natural Family Planning". Institute for Reproductive Health, Georgetown University. 2005. http://www.irh.org/nfp.htm. Retrieved 2008-05-18.
- ↑ Saint, Bishop of Hippo Augustine; Philip Schaff (Editor) (1887). A Select Library of the Nicene and Post-Nicene Fathers of the Christian Church, Volume IV. Grand Rapids, MI: WM. B. Eerdmans Publishing Co.. pp. On the Morals of the Manichæans, Chapter 18.
- ↑ 9.0 9.1 9.2 9.3 9.4 Green, Shirley (1972). The Curious History of Contraception. New York: St. Martin's Press. pp. 138–43. ISBN 0852230168.
- ↑ 10.0 10.1 McLaren, Angus (1992). A History of Contraception: From Antiquity to the Present Day. Oxford: Blackwell Publishers. p. 74. ISBN 0–631–18729–4.
- ↑ 11.0 11.1 Yalom, Marilyn (2001). A History of the Wife (First ed.). New York: HarperCollins. pp. 297–8, 307. ISBN 0-06-019338-7.
- ↑ "A Brief History of Fertility Charting". FertilityFriend.com. http://www.fertilityfriend.com/Faqs/A_brief_history_of_fertility_charting.html. Retrieved 2006-06-18.
- ↑ 13.0 13.1 Singer, Katie (2004). The Garden of Fertility. New York: Avery, a member of Penguin Group (USA). pp. 226–7. ISBN 1-58333-182-4.
- ↑ Gladwell, Malcolm (2000-03-10). "John Rock's Error". The New Yorker.
- ↑ "Basic Information on Natural Family Planning". United States Conference of Catholic Bishops. July 2007. http://www.usccb.org/prolife/issues/nfp/information.shtml.
- ↑ 16.0 16.1 Hatcher, RA; Trussel J, Stewart F, et al (2000). Contraceptive Technology (18th ed.). New York: Ardent Media. ISBN 0-9664902-6-6. http://www.contraceptivetechnology.com/table.html.
- ↑ 17.0 17.1 17.2 17.3 17.4 Kippley, p.154
- ↑ Arévalo M, Jennings V, Sinai I (2002). "Efficacy of a new method of family planning: the Standard Days Method." (PDF). Contraception 65 (5): 333–8. doi:10.1016/S0010-7824(02)00288-3. PMID 12057784. http://pdf.dec.org/pdf_docs/PNACQ416.pdf.
- ↑ "Perimon". 2007. http://www.perimon.com/en/. Retrieved 2007-02-11.
- ↑ "Safe Period Calculator". 2010. http://www.safe-period.com/. Retrieved 2010-07-22.
- ↑ Kalaca S, Cebeci D, Cali S, Sinai I, Karavus M, Jennings V (2005). "Expanding family planning options: offering the Standard Days Method to women in Istanbul.". J Fam Plann Reprod Health Care 31 (2): 123–7. doi:10.1783/1471189053629446. PMID 15921552.
- ↑ Urmil Dosajh, Ishita Ghosh, and Rebecka Lundgren (PDF). Feasibility of Incorporating the Standard Days Method into CASP Family Planning Services in Urban Slums of India. The Institute for Reproductive Health, Georgetown University. http://pdf.usaid.gov/pdf_docs/PNADG768.pdf. Retrieved 2006-12-02.
- ↑ Gribble J, Jennings V, Nikula M (2004). "Mind the gap: responding to the global funding crisis in family planning.". J Fam Plann Reprod Health Care 30 (3): 155–7. doi:10.1783/1471189041261483. PMID 15222918.
- ↑ Weschler, p.48.
- ↑ Kippley, p.111
- ↑ Kippley, pp.413-415
- ↑ Luc Bovens (2006). "The rhythm method and embryonic death" (PDF). Journal of Medical Ethics 32: 355–356. doi:10.1136/jme.2005.013920. http://jme.bmj.com/cgi/reprint/32/6/355.pdf.
- ↑ Gray, RH (October 1984). "Aged gametes, adverse pregnancy outcomes and natural family planning. An epidemiologic review". Contraception 30 (4): 297–309. doi:10.1016/S0010-7824(84)80022-0. PMID 6509983.
- ↑ Gray RH, Simpson JL, Kambic RT (May 1995). "Timing of conception and the risk of spontaneous abortion among pregnancies occurring during the use of natural family planning". American Journal of Obstetrics and Gynecology 172 (5): 1567–1572. doi:10.1016/0002-9378(95)90498-0. PMID 7755073.
- ↑ Barbato M, Bitto A, Gray RH, et al (June-September 1997). "Effects of timing of conception on birth weight and preterm delivery of natural family planning users". Advances in Contraception 13 (2-3): 215–228. doi:10.1023/A:1006508106197. PMID 9288339.
|
|||||||||||||||||||||||||||||||||||||
|
|||||||||||||||||||||||||||||||||||||||||||